It has been a very unique situation that we have faced over the last few months amidst this global pandemic COVID-19. With the recent phases of openings being put into action, Protege is prepared and Committed to the adherence of Ministry of Health guidelines, the Toronto Public Health unit and compliance of all legislation, including the Occupational Health and Safety Act, to assure that every measure will be taken to provide the public, student body and staff with the tools and direction for a safe return.
We like to take this opportunity to thank you for your continued patience as we go through this implementation process. Within this message are some key points for you to review to give you better insight into the virus, some FAQ’s, and to reduce the risk of transmission in our school, homes and community:
- What is COVID-19?
- How is it spread?
- How to Prevent the Spread?
- The Ministry of Health Screening Process
- Hand Sanitizing and Disposing Stations
- COVID-19: Have symptoms or been exposed?
- STEPS TO GET BETTER
- Reducing Social Stigmas and Discrimination associated with Covid-19
- Are you in crisis? If you're in immediate danger or need urgent medical support, call 911.
- COVID ALERT APP
- FAQ
What is COVID-19?
Coronaviruses (CoV) are a large family of viruses that cause illness ranging from the common cold to more severe diseases such as Middle East Respiratory Syndrome (MERS-CoV), Severe Acute Respiratory Syndrome (SARS-CoV), and COVID-19. A novel coronavirus is a new strain that has not been previously identified in humans. The number 19 refers to the year that the virus became active (2019)
How is it spread?
People can catch COVID-19 from others who have the virus. The disease spreads primarily from person to person through small droplets from the nose or mouth, which are expelled when a person with COVID-19 coughs, sneezes, or speaks. These droplets are relatively heavy, do not travel far and quickly sink to the ground. People can catch COVID-19 if they breathe in these droplets from a person infected with the virus. This is why it is important to stay at least 2 meters) away from others. These droplets can land on objects and surfaces around the person such as tables, doorknobs and handrails. People can become infected by touching these objects or surfaces, then touching their eyes, nose or mouth. This is why it is important to wash your hands regularly with soap and water or clean with alcohol-based hand rub.
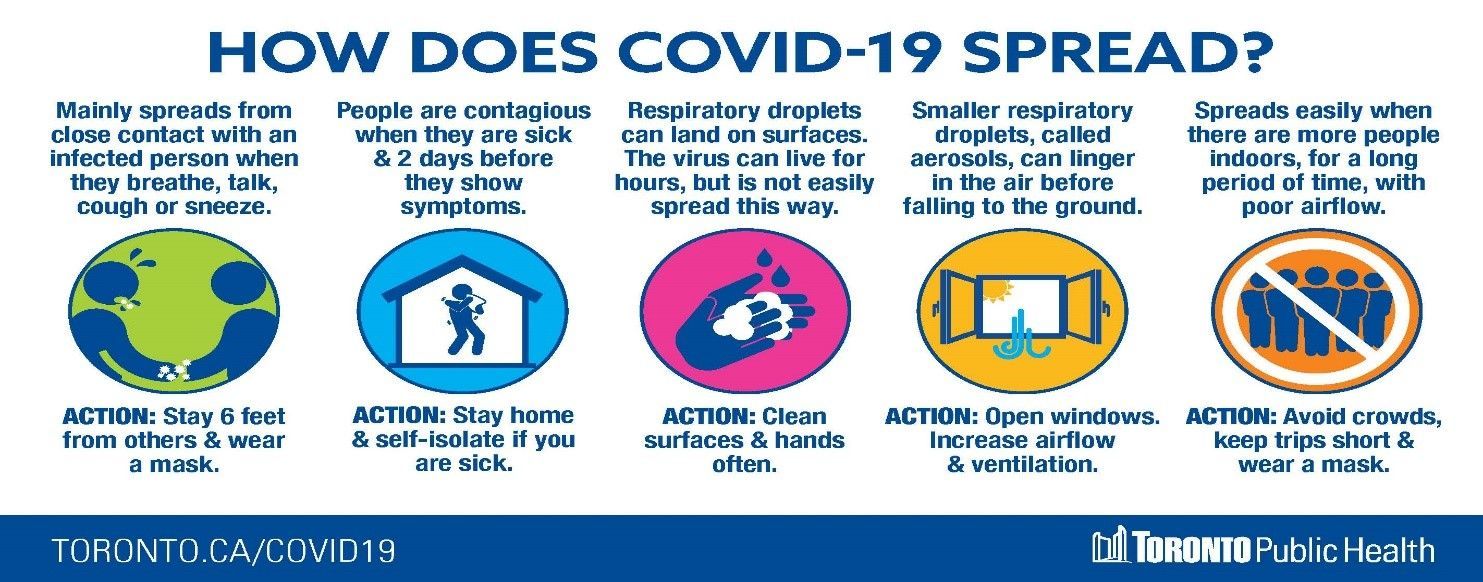
Causes infections of the nose throat and lungs and can be spread through:
- respiratory droplets generated when you cough or sneeze
- close, prolonged personal contact, such as touching or shaking hands
- touching something with the virus on it, then touching your mouth, nose or eyes before washing your hands.
How to Prevent the Spread?
Protégé encourages its community – including Students, staff, employees, volunteers, contractors, visitors and clients, anyone is eligible to receive a COVID-19 vaccine to get full vaccination by September 2021. Protégé will provide paid time off; assistance with booking vaccine appointment, peer-to-peer support for its employees, staffs and contractors and; assist students and volunteers for booking vaccine appointment and provide tutorial sessions for missing lectures due to vaccination.
- How to book a COVID-19 Vaccine Appointment - Ontario
- City of Toronto - COVID-19 - Protect Yourself and Others

- Download the COVID Alert app

- Recommend the app to others
- Recommendations and make informed decision on the use of COVID-19 Vaccine
- stay at home if you are sick
- avoid all non-essential trips or gatherings in your community
- do not gather in groups without mask
- limit contact with people at higher risk, such as older adults and those in poor health
- Always keep a distance of at least 2 arms lengths (approximately 2 meters) from others
- It is mandatory that you use a face covering to reduce the risk of transmission of COVID-19 when physical distancing and keeping two-meters’ distance from others may be challenging or not possible.
- Face coverings and face masks
- avoiding common greetings, such as handshakes
- wash your hands often with soap and water for at least 20 seconds
- use alcohol-based hand sanitizer if soap and water are not available
- when coughing or sneezing:
- cough or sneeze into a tissue or the bend of your arm, not your hand
- dispose of any tissues you have used as soon as possible in a lined waste basket and wash your hands afterwards
- avoid touching your eyes, nose, or mouth with unwashed hands.
- AVOID TOUCHING YOUR MASK!!!!
The Ministry of Health Screening Process
Screening questions will be asked of every person entering our facility to make sure to control any possible spread of the virus. These questions will be done both actively (prior to arrival to our facility) and passively (upon their arrival to our facility).
- Have you had close contact with anyone with acute respiratory Illness or travelled outside of Ontario in the past 14 days?
- Has there been any confirmed case of COVID-19 or had close contact with a confirmed case of COVID-19 in your household?
- Do you have any of the following symptoms?
- Fever > 37.8°C
- Cough
- Worsening chronic cough
- Shortness of breath
- Trouble breathing
- Sore throat or trouble swallowing
- Decrease or loss of sense of taste or smell
- Chills
- Headaches
- Unexplained fatigue, malaise, muscle (myalgias) or joint aches
- Nausea, vomiting, diarrhea, abdominal pain
- Pink eye (conjunctivitis)
- Runny nose, nasal congestion or stuffy nose
- Feeling unwell, very tired
- 70 years of age or older, are you experiencing any of the following symptoms: delirium, unexplained or increased number of falls, acute functional decline, or worsening of chronic conditions?
If the person answers YES to any of the above questions they are COVID Screen Positive and should get tested and be directed back to their local Public Health unit for further directions below COVID-19: Have symptoms or been exposed?
Resource:
COVID-19 Patient Screening Guidance Document
COVID-19: Have COVID-19 or Been Exposed
COVID-19 Test Locations: Ontario
Hand Wash, Hand Sanitizing and Disposing Stations
Protégé School has hand sanitizing stations available to the students and visiting public beyond all the cleaning areas we presently have. There are disposing area at these stations for masks and gloves. The directive for dealing with public and students before and after contact is to wash your hands thoroughly before and after the removal of any PPE that is being used.
We will have signage posted for proper hand washing, hand sanitizing, along with PPE recommended steps at every cleaning station.
Please Download Protégé Handwash Policy
COVID-19: Have symptoms or been exposed?
- Exposed to COVID-19 - If you have been in contact with someone who has tested positive for COVID-19 or has symptoms of COVID-19, you should:
- stay home and self-isolate for 14 days after your last contact with that person.
- monitor for symptoms of COVID-19.
- get tested

- Have Symptoms of COVID-19 - If you have symptoms of COVID-19, you must:
- stay home and self-isolate for 14 days after your symptoms started. After 14 days, you can stop isolating if you no longer have a fever and your symptoms have improved, but you should continue with physical distancing measures. If you are still unwell at 14 days, contact Telehealth or your health care provider.
- take steps to get better
- get tested
- Have COVID-19 - If you have tested positive for COVID-19, you must:
- self-isolate for 14 days after your symptoms started. After 14 days, you can stop isolating if you no longer have a fever and your symptoms have improved, but you should continue with physical distancing measures. If you are still unwell at 14 days, contact Telehealth or your health care provider.
- take steps to get better
STEPS TO GET BETTER
Monitor for the following symptoms for 14 days after exposure:
- Fever Cough
- Difficulty breathing
- Sore throat
- Runny nose
- Loss of taste or smell
- Nausea, vomiting, diarrhea
- Difficulty swallowing
Disease symptoms may be different, depending on age. Children and older adults with COVID-19, may also have non-specific symptoms, such as:
- Disorientation, confusion
- Sleeping more than usual or muscle aches
- Dizziness, weakness or falls
- Chills, headache
During this time limit contact with others, wear a mask or face covering and continue to follow all Hand Hygiene Protocols. If you develop symptoms self isolate immediately.
Self- Isolate and contact Telehealth at 1-866-797-0000
Stay home
- Do not go outside, unless on to a private balcony or private enclosed yard where you can avoid close contact with others.
- Do not use public transportation, taxis or ride-shares.
- Shop online or have a friend or family member pick up supplies for you.
Avoid contact with others
- Do not have visitors unless essential (e.g. care providers).
- Stay away from seniors and people with chronic medical conditions (e.g. diabetes, lung problems, immune deficiency).
- As much as possible, stay in a separate room from other people in your home and use a separate bathroom if you have one.
- If you have to be in contact with others, practise physical distancing and keep at least two metres/six feet between yourself and other people.
- Make sure that shared rooms have good airflow (e.g. open windows).
Cover your coughs and sneezes
- Cover your mouth and nose with a tissue when you cough or sneeze.
- Throw used tissues in a wastebasket lined with a plastic bag, and clean your hands.
- Clean your hands after emptying the wastebasket.
- If you do not have a tissue, cough or sneeze into your upper sleeve or elbow, not your hand.
Clean your hands
- Clean your hands often with soap and water and lather for at least 15 seconds.
- Dry your hands with a paper towel, or with your own cloth towel that no one else shares.
- Use alcohol-based hand sanitizer (70-90% alcohol concentration) if your hands are not visibly dirty.
- Avoid touching your eyes, nose, and mouth with unclean hands.
Wear a mask over your nose and mouth
- Wear a mask if you must leave your house to see a health care provider.
- Wear a mask if you are within two metres/six feet of other people, or stay in a separate room.
- Ensure your mask completely covers your nose and mouth and make sure there are no gaps between your face and the mask.
- If a medical mask is not available, a non-medical mask or face covering (e.g. homemade cloth mask, dust mask, bandana, or scarf) can be worn.
- If you cannot wear a mask, people should wear a mask when they are in the same room as you.
Clean your home
- Clean your home with regular household cleaners.
- Clean frequently touched items such as toilets, sink tap handles, doorknobs and bedside tables on a daily basis.
Avoid sharing household items
- Do not share dishes, drinking glasses, cups, eating utensils, towels, bedding or other items with others.
- After use, these items should be washed with soap or detergent in warm water. No special soap is needed.
- Dishwasher and washing machines can be used.
- Do not share cigarettes.
Monitor your symptoms
- If you develop symptoms or your symptoms are worsening, and you are concerned, contact Telehealth at 1-866-797-0000 or your health care provider.
- If you need urgent medical attention, contact 911.
Travel to and from the hospital or health care provider’s offic
- Do not use public transportation.
- Drive yourself if possible.
- If driving yourself is not possible, arrange a ride with a family member, friend, taxi, or ride share. Sit in the back seat, open the window, and wear a mask.
- If you take a taxi/ride share, record company name and operator number
- International students will have accommodations made in this circumstance
Inform your contacts if you have symptoms of COVID-19
- Please inform anyone who lives in your household and anyone else you had close contact with to isolate for 14 days from the last day they had contact with you.
- Inform Protégé School 416-754-9866
- This applies to anyone you had close contact with up to 48 hours before you were sick and while you were sick.
When to end self-isolation
- If you had symptoms:
- Isolate for 14 days beginning when your symptoms started.
- After 14 days, you can stop isolating if you no longer have a fever and your symptoms have improved, but you should continue with physical distancing measures. If you are still unwell at 14 days, contact Telehealth or your health care provider.
- If you did not have COVID-19 symptoms but were tested:
- Follow the advice of public health
- If you had contact with someone with COVID-19 or COVID-19 symptoms:
- Isolate for 14 days after your last contact with that person.
Treatment - There is no specific treatment for COVID-19. People who have COVID-19 should receive supportive health care to help relieve symptoms. People with more severe illness may require hospitalization.
- If symptoms feel worse than a standard cold, call your health care practitioner. They can relieve symptoms by prescribing a pain or fever medication.
- You should also:Drink plenty of fluids
- Get rest and sleep as much as possible
- Try a humidifier or a hot shower to help with a sore throat or cough
Get Tested
- There is a test for COVID-19. The test tells you if you have the infection right now. The test involves taking a swab from the back of the nose or throat.
- You should get tested for COVID-19 if:
- You have one or more symptoms of COVID-19, even if they are mild.
- Some asymptomatic individuals may be recommended for testing in consultation with public health. This includes if:
- You were a close contact of someone who has COVID-19;
- You are concerned you may have been exposed to someone who might have COVID-19, even if you do not have symptoms;
- To get tested, find an assessment centre in Toronto.
- Results can take up to four days.
- You may contact Toronto Public Health at 416-338-7600.
- Individuals without a health card must follow up with the assessment centre or testing physician directly for lab results.
- If you were not tested but you have symptoms of COVID-19, please inform anyone you had close contact with to self-isolate for 14 days from the last day they had contact with you. This applies to people who live in your household and to anyone else you had close contact with while you were sick and not self-isolating, and up to 48 hours before you were sick.
Contacted by Toronto Public Health, you may be contacted by Toronto Public Health if you may have been exposed to COVID-19.
- Cases and suspected cases of COVID-19 are reportable to local health authorities under the Provincial Health Protection and Promotion Act . As Toronto Public Health is notified of potential cases, they are immediately following up directly with the individuals to let them know.
- Please follow the directions given to you by Toronto Public Health or health authorities.
Return to School
- There are no tests to do to be cleared to return to school.
- In general, one can return 14 days after their symptoms began if they had COVID-19.
- For other illnesses, or if someone tested negative for COVID-19, they should not return to work until they are symptom-free for at least 24 hours
Reducing Social Stigmas and Discrimination associated with Covid-19
COVID-19: Testing and reducing stigma
WHAT IS SOCIAL STIGMA?
Social stigma in the context of health is the negative association between a person or group of people who share certain characteristics and a specific disease. In an outbreak, this may mean people are labelled, stereotyped, discriminated against, treated separately, and/or experience loss of status because of a perceived link with a disease. Such treatment can negatively affect those with the disease, as well as their caregivers, family, friends and communities. People who don’t have the disease but share other characteristics with this group may also suffer from stigma. The current COVID-19 outbreak has provoked social stigma and discriminatory behaviours against people of certain ethnic backgrounds as well as anyone perceived to have been in contact with the virus.
WHAT IS THE IMPACT?
Stigma can undermine social unity and persuade social isolation of groups, which might contribute to a situation where the virus is more, not less, likely to spread. This can result in more severe
health problems and difficulties controlling a disease outbreak. Stigma can:
- Drive people to hide the illness to avoid discrimination
- Prevent people from seeking health care immediately
- Discourage them from adopting healthy behaviours
HOW TO ADDRESS SOCIAL STIGMA?
Evidence clearly shows that stigma and fear around communicable diseases delay the response. What works is:
- Building trust in reliable health services by providing accurate and consistent information and updated advice
- Showing empathy and encouragement with those affected. Sharing stories and experiences humanizes the struggles by individuals and groups.
- Understanding the disease itself and spread the facts. Correct misconceptions and challenge the myths and stereotypes Coronavirus disease (COVID-19) advice for the public: Mythbusters
- Adopting effective, practical measures people can help to keep loved ones safe as well as promoting the importance of prevention, life saving actions, early screening and treatment
- Take care of your mental and physical health during the COVID-19 pandemic Taking care of your mental and physical health during the COVID-19 pandemic
- Creating an environment where the impact of the disease can be addressed openly, honestly and effectively
- When talking about coronavirus disease, certain words and language may have a negative meaning for people and fuel stigmatizing attitudes
- Choose a “language” or choice of words that respects and empowers people
- Below are some dos and don'ts on language when talking about the new coronavirus disease (COVID-19):
-
- DO'S
- DON'T'S
-
-
DO
Talk about the new coronavirus disease (COVID-19)
-
Don't
attach locations or ethnicity to the disease, this is not a "Wuhan Virus", "Chinese Virus", or "Asian Virus".
The official name for the disease was deliberately chosen to avoid stigmatization - the"co" stands for Corona, "vi" for virus and "d" for disease, 19 is because the disease emerged in 2019.
-
-
-
DO
talk about "people who have COVID-19", "people who are being treated for COVID-19", "people who are recovering from COVID-19&" or "people who died after contracting COVID19"
-
Don't
refer to people with the disease as "COVID-19 cases" or "victims"
-
-
-
DO
talk about "people who may have COVID-19" or "people who are presumptive for COVID-19"
-
Don't
talk about “COVID-19 suspects” or “suspected cases”
-
-
-
DO
talk about people “acquiring” or “contracting” COVID-19
-
Don't
talk about people “transmitting COVID-19” “infecting others” or “spreading the virus” as it implies intentional transmission and assigns blame. Using criminalizing or dehumanizing terminology creates the impression that those with the disease have somehow done something wrong or are less human than the rest of us, feeding stigma, undermining empathy, and potentially fueling wider reluctance to seek treatment or attend screening, testing and quarantine.
-
-
-
DO
speak accurately about the risk from COVID-19, based on scientific data and latest official health advice.
-
Don't
repeat or share unconfirmed rumours, and avoid using hyperbolic language designed to generate fear like “plague”, “apocalypse” etc.
-
-
-
DO
talk positively and emphasize the effectiveness of prevention and treatment measures. For most people this is a disease they can overcome. There are simple steps we can all take to keep ourselves, our loved ones and the most vulnerable safe.
-
Don't
emphasize or dwell on the negative, or messages of threat. We need to work together to help keep those who are most vulnerable safe.
-
-
-
DO
emphasize the effectiveness of adopting protective measures to prevent acquiring the new coronavirus, as well as early screening, testing and treatment.
-
-
https://www.who.int/docs/default-source/coronaviruse/covid19-stigma-guide.pdf?sfvrsn=226180f4_2
FEELING ANXIOUS ABOUT COVID-19? Fear, stress and worry are normal in a crisis
The COVID-19 pandemic has resulted in many changes. You might feel like you're no longer in control of things. It’s normal to feel sad, stressed, confused, scared or worried. People react in different ways. Some common feelings include:
- a sense of being socially excluded or judged
- concern about your children's education and well-being
- fear of getting sick with COVID-19 or of making others sick
- worry about losing your job, not being able to work or finances
- fear of being apart from loved ones due to isolation or physical distancing
- helplessness, boredom, loneliness and depression due to isolation or physical distancing
Tips for taking care of yourself
- Stay informed but take breaks from social media and the news.
- Practise physical distancing, but stay socially connected to friends and family through:
- Phone calls
- Video chats
- Social media
- Practise mindfulness by:
- Stretching
- Meditating
- Taking deep breaths
- Try to
- Eat healthy meals
- Exercise regularly
- Get plenty of sleep
- Follow safe food handling and cooking practices to keep you and your family safe by killing the virus and lowering your risk of infection.
- Think about how to use any unexpected flexibility in your daily routine.
- Focus on the positive aspects of your life and things you can control.
- Be kind and compassionate to yourself and others.
- If you can, limit your use of substances.
- If you do use substances, practise safer use and good hygiene.
Are you in crisis? If you're in immediate danger or need urgent medical support, call 911.
If you're experiencing gender-based violence, you can access a crisis line.
Assaulted Women's Helpline
- Toll free: 1-866-863-0511 (multilingual services available)
- Toll free TTY: 1-866-863-7868
- or #SAFE (#7233) on your Bell, Rogers, Fido or Telus mobile phone
Talk4Healing
- Toll free: 1-855-554-4325 (multilingual services available)
You may also access support workers, social workers, psychologists and other professionals for confidential chat sessions or phone calls by texting WELLNESS to:
- 686868 for youth
- 741741 for adults
COVID ALERT APP
The Government of Canada has asked telecommunication providers to help spread the message about their new COVID Alert app.
- Download the COVID Alert app for free, and help protect yourself and your community. The COVID Alert app lets users know if they have been exposed to COVID-19.
- Available now in Ontario in the Apple App Store or Google Play.
FAQ
Are Protégé students providing treatment to the public?
Currently Protégé School will not involve an immediate return to practice on the public. Please visit our website regularly for any updates on the re-opening of student clinic or call the school to verify. Please do not come without a scheduled appointment as we are NOT ACCEPTING WALK-INS at this time.
Are students required to wear masks while taking part in practical/treatment?
Yes, Students and Instructors are required to wear surgical/procedure masks while within two meters of clients including while providing treatment. Masks are not to be touched while wearing and must be changed whenever wet, damaged or soiled. Hands must be washed before and after touching, adjusting, putting on, or removing the masks.
Are clients required to wear masks during treatment? What if they refuse?
In accordance with the Ontario Ministry of Health’s recommendation to wear masks whenever physical distancing is not possible, clients are instructed to come to the appointment wearing a clean disposable or clean reusable mask to be worn throughout the treatment.
The student may need to make practice modifications to accommodate and facilitate the ability of clients to wear masks throughout treatment. Client safety and comfort during treatment must be prioritized. If the client cannot wear a mask (e.g. due to a health condition or difficulty breathing), the student along with the supervisor will use their professional judgement to assess the risk of providing or continuing treatment. If it is deemed unsafe to provide treatment without the client wearing a mask, the student/supervisor can refuse to treat the client and clearly document this in the client health record.
What types of gloves are acceptable?
Students do not need to use gloves for most treatments. Glove use is not a substitute for proper hand washing. Hand washing is an extremely important measure in preventing the spread of COVID-19. Gloves provided by Protégé meet the requirements put forth as acceptable PPE should the need for gloves were to arise.
What type of cleaning and disinfecting agents is Protégé School using?
Protege School uses decontaminating products and procedures approved by Health Canada. Disinfection of high touch areas and including study and practical settings will be thoroughly disinfected as per Public Health and Safety protocol.
Health Canada has released a list of approved products for the purpose of cleaning and disinfecting. We will continue to use and maintain our high standard of cleaning and disinfection of porous items such as massage tables and pillow covers and porous items with Genie-Plus. For hard non-porous surfaces, we will continue to use Pre-empt Cs20. Bleach Solutions and 70% Isopropyl Alcohol.
A list of approved hard surface disinfectants can be found: List of disinfectants with evidence for use against COVID-19




